
Calcium: The essential mineral
What is calcium and what does it do?
Calcium is the most abundant mineral in the body and an essential micronutrient, which should be provided by the diet. A mature body contains about 1000 g of calcium, 99% of which is found in the bones, where it forms part of the rigid skeletal structure and serves as a mineral reservoir for the blood. The residual 1% is found in extracellular fluids, intracellular structures and cell membranes, where vitamin D and the action of hormones (parathyroid hormone and calcitonin) facilitate its role in muscle contraction, blood clotting, neural transmission and regulating blood pressure.1-3 Apart from its physiological functions and the role in maintaining bone health, calcium has also been shown to have a role in the prevention and treatment of cardiovascular disease, certain cancers and weight management.
The body’s need for calcium varies owing to relative skeletal growth and remodelling in different life stages. Calcium is critically important for bone accretion during skeletal growth and maintenance of bone mass after growth is completed. Net calcium is lost from the body when bone formation no longer keeps up with bone resorption during late adulthood.3
Obligatory losses of calcium that occur through urine, faeces and the skin range from 150 to 300 mg/day. These requisite losses, together with the physiological requirements for growth, can be balanced only by sufficient dietary calcium intake. If dietary calcium is inadequate, calcium is taken from the bone through the interaction of the main calcium-regulating hormones.1,2,4 The serum calcium concentration, which is tightly regulated at 2.25-2.60 mmol/L by means of homeostatic control, is therefore maintained at the expense of bone.
Calcium from food
Calcium cannot be synthesized by the body and thus has to be obtained from food. Dairy products are the richest food source of calcium, although foods such as sardines, tofu (fortified with calcium), beans (red, white), certain fruit (e.g. figs) and vegetables (e.g. spinach, sweet potato and broccoli), almonds and salmon also contain calcium.5,6
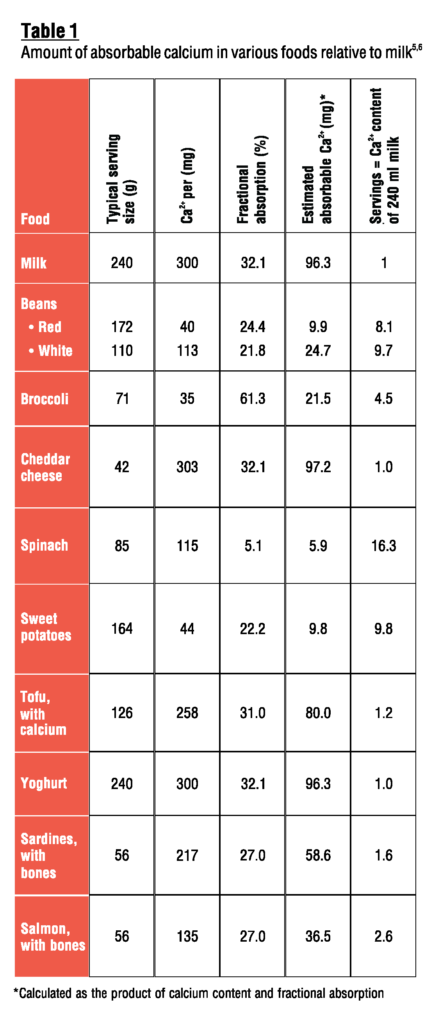
Calcium from dairy products is well absorbed (22-27%).4 The amount of absorbable calcium found naturally in various food sources is compared with that of milk in Table 1. Apart from having a high total calcium content, milk and dairy products are also unique sources of calcium owing to the ratio of calcium to protein and calcium to phosphorus. 7
Various non-dairy beverages, also called milk alternatives, are used as proposed substitutes to cow’s milk. These include ‘milk’ made from almonds, cashews, coconut, hazelnuts, oats, rice and soy. Most of these beverages are fortified with calcium to imitate the calcium levels in cow’s milk. However, except for fortified soy milk, the bioavailability of calcium in these beverages is mostly unknown.8
Calcium-fortified soy milk (containing tricalcium phosphate at 300 mg/serving) was not found to be comparable to cow’s milk as calcium source, as intrinsically labelled calcium was found to be absorbed at only 75% of that of cow’s milk.9 In contrast, comparable amounts of calcium were found to be absorbed from soy milk fortified with a proprietary phosphate of calcium when compared with cow’s milk.10 These non-dairy beverages should, however, not be considered equivalent nutritional substitutes to cow’s milk until their nutritional quality and bioavailability have been established.8
Calcium absorption
Calcium is absorbed primarily in the duodenum by an active transcellular and saturable system, which is stimulated and regulated by vitamin D, and through passive and vitamin D-independent paracellular transport in the jejunum and ileum. When calcium intake is high, some absorption (about 4%) even occurs in the colon.4
Calcium absorption increases when the need in the body increases and when dietary intakes are low or inadequate. Newborn infants absorb 55-60% of the calcium they consume, while growing children and teenagers absorb up to 50% and adults only 30% on average.1 Calcium absorption decreases with age and does not adapt to a low intake in the same way as during the younger years. A negative calcium balance is therefore more easily seen in the elderly than in younger subjects in case of low intakes.4
The bioavailability of calcium from food
The bioavailability of calcium is defined as the fraction of dietary calcium that can potentially be absorbed from the intestine and be used for physiological functions (particularly bone mineralization) or to limit bone loss.11 In contrast, absorbability depends on the components of the given food item.12 One of the strategies to optimize calcium intake is to increase the availability of calcium from foods. Calcium absorption and bioavailability are influenced by both endogenous factors (age, physiological condition and hormonal regulation) and exogenous factors, which affect the relative absorption or excretion of calcium.
Dietary factors influencing intestinal absorption of calcium
Owing to its association with phytates, fibre is negatively linked with calcium absorption, although fibres alone (e.g. cellulose, hemicellulose, lignin and non-cellulose polysaccharides) seem to have no direct effect on calcium absorbability.11
Food constituents such as phytates (found in wheat bran, beans, seeds, nuts, soy isolates and fibre-containing wholegrain products), oxalates (found in spinach, nuts, cabbage, sweet potatoes, rhubarb and beans) and tannins (tea) can reduce calcium absorption by forming insoluble complexes. However, calcium balance seems to be affected by these food constituents only if the diet is unbalanced (e.g. when consuming a strict vegetarian diet, which is high in fibre but lacks dairy products and their associated calcium).11
Non-digestible oligosaccharides (inulin, fructans, etc.) are partially or totally fermented in the large intestine, leading to the production of short-chain fatty acids. This stimulates calcium absorption owing to the acidification of the intestine.13
Vitamin D assists in maintaining an optimal calcium blood concentration by increasing calcium absorption from the digestive tract, withdrawing calcium from bones and stimulating retention by the kidneys.1 Insufficient vitamin D levels due to inadequate dietary intake and sun exposure therefore also interfere with calcium absorption.14
Phosphopeptides (derived from the enzymatic hydrolysis of caseins) have a positive effect on calcium absorption through facilitating its absorption by passive diffusion.11
Lactose facilitates calcium absorption by stimulating, independently from vitamin D, the diffusive system from intestinal calcium transfer.7
Dietary factors influencing the excretion of calcium in urine
Certain anions, such as sulfate and chloride, organic ligands (chelators) and excess protein or sodium all increase urinary loss of calcium and therefore hinder its incorporation into bone.5 The renal excretion of calcium increases by an average of 30-40 mg for every 2 g of sodium intake; however, a sodium intake below 2400 mg/day will not negatively impact bone health.12,14
The increases in urinary calcium excretion associated with high-protein diets do not seem to be linked to an impaired calcium balance and so have no detrimental effect on bone health. In fact, data from a systematic review by Calvez et al.13 indicate that high protein intakes induce an increase of intestinal calcium absorption, promote bone growth and retard bone loss. The presence of phosphorus also decreases urinary calcium losses by 40-65% depending on the level of protein intake, thereby counteracting the hypercalciuretic effect of protein intake.
Phosphorus may affect the urinary excretion of calcium directly, by increasing its reabsorption in the distal part of the nephron or enhancing the uptake of absorbed calcium into bone, or indirectly, by stimulating secretion of parathyroid hormone. The simultaneous absorption of calcium and phosphorus increases the uptake of calcium by bone, thereby decreasing its loss in urine.11
Sulfate ions also bind calcium, preventing its tubular reabsorption and even its incorporation into bone. Chronic metabolic acidosis due to excessive intakes of sulfate and chloride anions leads to higher urinary calcium losses.11
Dietary factors affecting the amount of calcium lost in the urine have major influences on calcium balance. However, calcium recommendations are calculated to take most of these losses into account.11
Conclusion
Milk and other dairy products should be part of everyone’s daily diet in order to meet calcium recommendations for good health, especially with regard to optimal skeletal development and maintenance of bone health. As milk supplies calcium that is well absorbed and supports long-term bone health, it presents the most suitable dietary constituent for achieving optimal calcium intake.
References
- Whitney E, Rolfes SR. Understanding nutrition. 14th ed. Stamford: Cengage Learning; 2016.
- EFSA Panel on Dietetic Products, Nutrition and Allergies. Scientific opinion on dietary reference values for calcium. EFSA J. 2015; 13(5):4101. doi:10.2903/j.efsa.2015.4101
- Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: National Academies Press; 2011.
- Burckhardt P. Calcium revisited: Part I. Bonekey Rep. 2013; 2:433. doi:10.1038/bonekey.2013.167
- Weaver CM, Proulx WR, Heaney R. Choices for achieving adequate dietary calcium with a vegetarian diet. Am J Clin Nutr. 1999; 70(3 Suppl):543S-548S.
- Titchenal CA, Dobbs J. A system to assess the quality of food sources of calcium. J Food Compos Anal. 2007; 20:717-724.
- Klobukowski JA, Skibniewska KA, Kowalski IM. Calcium bioavailability from dairy products and its release from food by in vitro digestion. J Elem. 2014; 19(1):277-288.
- Singhal S, Baker RD, Baker SS. A comparison of the nutritional value of cow’s milk and nondairy beverages. J Pediatr Gastroenterol Nutr. 2017; 64(5):799–805.
- Heaney RP, Dowell MS, Rafferty K, Bierman J. Bioavailability of the calcium in fortified soy imitation milk, with some observations on method. Am J Clin Nutr. 2000; 71:1166-1169.
- Tang AL, Walker KZ, Wilcox G, Strauss BJ, Ashton JF, Stojanovska L. Calcium absorption in Australian osteopenic postmenopausal women: An acute comparative study of fortified soymilk to cows’ milk. Asia Pac J Clin Nutr. 2010; 19(2):243-249.
- Guéguern L, Pointillart A. The bioavailability of dietary calcium. J Am Coll Nutr. 2000; 19(2 Suppl):119S-136S.
- Burckhardt P. Calcium revisited, part III: Effect of dietary calcium on BMD and fracture risk. Bonekey Rep. 2015; 4:708. doi:10.1038/bonekey.2015.77
- Calvez J, Poupin N, Chesneau C, Lassale C, Tomé D. Protein intake, calcium balance and health consequences. Eur J Clin Nutr. 2012; 66(3):281-295.
- Pereira GAP, Genaro PS, Pinheiro MM, Szejnfeld VL, Martini LA. Dietary calcium – strategies to optimize intake. Rev Bras Reumatol. 2009; 49(2):164-180.


